I have spent two years, studying the work of experts in the field of autoimmunity and have combined what I’ve learned, in 24 steps. I’ll be sharing one step every week for the next 24 weeks, on my website and social media platforms (starting Monday 18 May 2020). This is step 9 of 24.
Facebook: Autoimmune Way
Instagram: Autoimmune Way
STEP 9: HEALING THE GUT
GUT HEALTH
We now know that 80% of the immune system is located in the gut. This means that if you don’t have a healthy gut, you won’t have a healthy immune system. Gut health is a critical step in healing and recovering from autoimmunity even if your condition is not directly linked to your gut. For example, there is not doubt that ulcerative colitis is linked to your gut but not everyone would link rheumatoid arthritis to your gut health.
The gut is a complex system that includes every part of your body involved in digestion. So, what does it mean to have good gut health? You know you have good gut health if:
- You feel good after eating.
- You have one to three bowel movements per day.
- You do not struggle with bloating, cramps or pain after eating.
- You don’t have undigested food in your stool.
- You don’t use or need digestive medications.
- You don’t have acid reflux.
So, let’s look at the flip-side, how do you know you have poor gut health.
You know you have poor gut health if you struggle with:
- Acne
- ADD/ADHD
- Anxiety
- Arthritis
- Asthma
- Autoimmunity
- Belching
- Bloating
- Brain fog
- Chronic coughing
- Chronic fatigue
- Congestion
- Constipation
- Depression
- Diarrhea
- Dizziness
- Fibromyalgia
- Frequent illness
- Headaches
- Heartburn
- Hormone imbalance
- Insomnia
- Intestinal spasms
- Joint pain
- Low white blood count
- Mood swings
- Nausea
- Vomiting
- Passing gas
- Seasonal allergies
- Skin rashes
- Eczema
- Hives
- Rosacea
- Stomach pain
- Stuffy nose
- Thyroid imbalance
- Weight gain
- Inability to lose weight
UNDERSTANDING THE ROLE THE GUT MICROBIOME PLAYS
Bacteria, viruses, fungi and other microscopic living things are referred to as microorganisms, or microbes, for short. Trillions of these microbes exist mainly inside your intestines and on your skin. Most of the microbes in your intestines are found in a “pocket” of your large intestine called the cecum, and they are referred to as the gut microbiome. Although many different types of microbes live inside you, bacteria are the most studied.
In fact, there are more bacterial cells in your body than human cells. There are roughly 40 trillion bacterial cells in your body and only 30 trillion human cells. That means you are more bacteria than human. What’s more, there are up to 1,000 species of bacteria in the human gut microbiome, and each of them plays a different role in your body. Most of them are extremely important for your health, while others may cause disease.
These microbes have co-evolved with humans, depending on us for their survival just as we depend on them for our health and well-being. For example, we provide nutrients for bacteria which then keep our immune system in check, digest certain carbohydrates that would be indigestible to us, and make vitamins and other important compounds that we would otherwise be unable to produce. This wonderful, symbiotic relationship is what makes up your microbiome.
The gut microbiome begins to affect your body the moment you are born. You are first exposed to microbes when you pass through your mother’s birth canal. However, new evidence suggests that babies may come in contact with some microbes while inside the womb. As you grow, your gut microbiome begins to diversify, meaning it starts to contain many different types of microbial species. Higher microbiome diversity is considered good for your health.
The gut microbiome affects the body from birth and throughout life by controlling the digestion of food, immune system, central nervous system and other bodily processes.
An imbalance of healthy and unhealthy microbes is called gut dysbiosis. When the normal gut microbial communities are disturbed, for various reasons (like using antibiotics or suffering from a bacterial infection), it can lead to gut dysbiosis. Dysbiosis is associated with a growing number of diseases such as Crohn’s disease, ulcerative colitis, irritable bowel syndrome, and both type 1 and type 2 diabetes. You’ll find that the variety and balance of gut bacteria is often different in people with chronic inflammatory conditions as compared with healthy individuals.
Research now suggests that these diseases are not due to any single bacterium, but from changes to the entire microbiome. And since a large part of our immune system is found within the gut, several diseases resulting from dysbiosis are autoimmune diseases.
Dr Amy Myers explains it beautifully. She likes to think of the gut microbiome as a rainforest. In a rainforest, many types of plants live together in a symbiotic ecosystem but if the balance gets disrupted, the good or beneficial plants begin to die and the bad ones start to take over. This also happens in your gut– even just one dose of antibiotics can throw off the balance of the good bacteria that used to keep your immune system running optimally. The good gets killed or greatly reduced, and the bad bacteria (SIBO) and yeast (Candida) that used to be kept in check can take over and grow out of control.
Additionally, if you’re eating a diet high in refined carbohydrate, sugar and alcohol then you will feed the SIBO and yeast (Candida), letting them grow even more out of control. Certain medications such as antibiotics, acid blocking drugs, birth control pills and steroid can also cause further dysbiosis. As the dysbiosis gets more out of control it can cause a suppression in your immune system – remember 80% of your immune system is in the gut – which then can lead to being susceptible to other infections which may require more antibiotics and the cycle just keeps going.
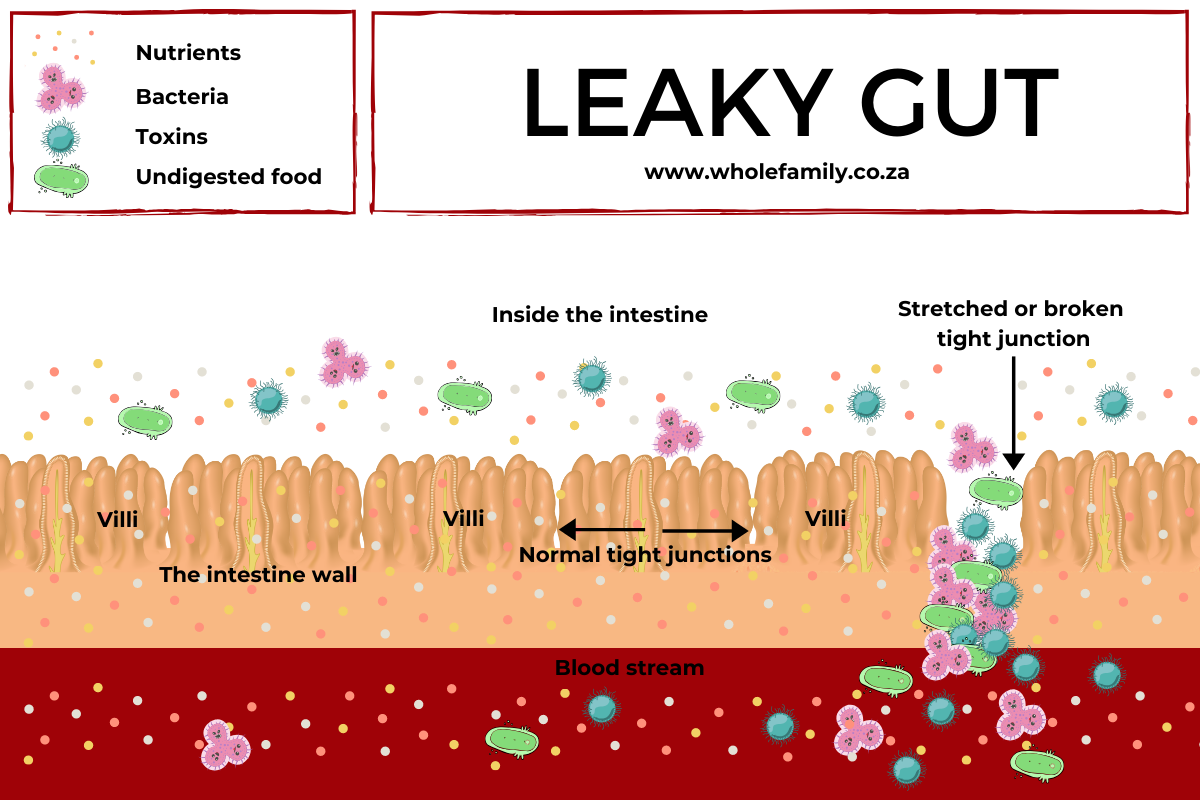
Over time, having this dysbiosis in your gut microbiome will eventually lead to a leaky gut.
According to Chris Kresser, M.S. many autoimmune diseases are being studied to look for gut dysbiosis, providing increasing evidence that disruption of the microbiome is associated with the development of some autoimmune diseases. Though there is clear correlation between changes in the microbiome and autoimmune disease, it is not clear if it is the dysbiosis that leads to autoimmune disease, or if dysbiosis is the result of an overactive and misdirected immune system.
UNDERSTANDING THE ROLE LEAKY GUT PLAYS
If you have been following the 24 steps to reclaiming your life from Autoimmunity, you would know what leaky gut is (step 6) and understand the role it plays in your autoimmune disease. I encourage you to revisit step 6, to get a better understanding of leaky gut.
HEALING THE GUT
Functional medicine has developed a very effective method of healing and protecting your gut. The method is called the 5R’s and consists of the following steps:
- Remove the bad
- Replace with the good
- Reinoculate with healthy bacteria
- Repair the gut
- Rebalance
The 5R’s of healing the guts will be explored in steps 10 – 14.
I invite you to join the Autoimmune Way program to learn how to heal your gut.